Huggies Diarrhoeal dehydration article by Lynne Bluff

On a daily basis it is stressful being a parent even when your child is healthy and well. Many parents want to be given exact instructions on what to do when, when their baby / toddler / child becomes not well. Well, this just isn’t possible – every baby is different and needs to be looked at individually. There certainly are some guidelines we can give you to assist in caring for your little one and making the all-important decision of when to go to the doctor. It is also about knowing how to get through a trying period of an illness when help may not be close at hand - but if you know what to do – you can see you and your little one successfully through a crisis.
Note – this article is here to give you some guidance. This information does not constitute medical advice. If you are concerned about your baby / toddler / child’s condition – please seek medical help immediately!
So, what is diarrhoea?
Diarrhoea is the correct name for loose/liquid stools or poos. (it is commonly referred to as a runny tummy). Diarrhoea is often liquid in consistency and passed in more profuse volumes than normal. It is important to know the difference between diarrhoea and a normal breastfed stool. A normal breastfed poo is very soft in consistency and can be passed in large volumes. The reassuring thing about this is if you are breastfeeding your baby – they are less likely to end up with diarrhoea as breast milk has anti-infective properties in it.
Diarrhoea is generally classified as 3 or more loose / liquid stools in a day (it can be a lot more too). An increase in volume, an increase in wateriness and an increase in frequency.
Thankfully the majority of cases of diarrhoea are mild and easily rectified. However, it can be serious and have very serious implications. The problem with diarrhoea is if your little one becomes dehydrated (more fluid is coming out of the body than going in). Particularly in young babies and children, dehydration can be life-threatening, so we always need to stay alert and in-touch with our little one.
Causes of diarrhoea
-
Most commonly diarrhoea is caused by viral gastroenteritis. Gastroenteritis is an infection in the bowel. The most common viruses are rotavirus, norovirus and adenovirus. These viral infections are very infectious and can be easily and quickly spread. It can start off with vomiting and a slight fever.
-
Bacterial gastroenteritis – is caused by bacteria like salmonella, shigella etc – these are often linked to food poisoning. It comes on suddenly and can cause blood and mucous in the stool.
-
The after-effects of a course of antibiotics can cause diarrhoea as the antibiotics have wiped out the good bacteria in the bowel and it becomes overrun with the wrong microorganisms.
-
Lactose intolerance can cause diarrhoea as well – when your baby is reacting to the sugar - lactose that is found in milk.
-
Drinking too much fruit juice can result in diarrhoea.
When looking at any illness your baby has and when to go to the doctor. Look at your baby as a whole “package” – so don’t just look at what he is drinking, or how many dirty / wet nappies he is having but put all this together and look at your baby as a complete entity. Also to assess how sick your child is – look at your baby’s personality – is my baby the same content, happy, smiley baby as normal. Or is my baby sleepy and lethargic? Or, is my baby an unhappy, crying baby? This observation goes a long way to assess how sick your baby is.
The second important thing is to try to stay calm. When we are anxious and uptight, our babies’ sense this and pick up our stresses and start to mirror our emotions. So, stay calm and in control to make a good assessment of your little one.
Some key facts according to the WHO (World Health Organisation)
-
Diarrhoeal disease is the third leading cause of death in children 1-59 months of age. It is both preventable and treatable
-
Each year diarrhoea kills about 443 832 children under the age of 5
-
Globally, there are 1,7 billion cases of childhood diarrhoeal disease each year
Can diarrhoea in children be prevented?
Minimise the spread of gastroenteritis by
-
washing hands regularly, particularly
-
after changing nappies,
-
going to the toilet,
-
before and after preparing food
-
-
Make sure your child is vaccinated against Rotavirus – this decreases the risk of your baby being hospitalised due to diarrhoea. (This should be given at 6, 10 and 14 weeks of age. (There are to vaccine options in SA).
-
Follow good food safety practices
-
Keep your child at home if he has diarrhoea.
The positive aspect of diarrhoea is that it is preventable and treatable.
The biggest problem with diarrhoea is it leads to dehydration. So, know what to look for and how to treat it – and you will be doing a great job!
The signs of dehydration
-
If your toddler is excessively thirsty – they may already be dehydrated
-
Little or no urine for 6-8 hours
-
Urine is dark – check out the urine colour chart to assess dehydration
-
Dry skin
-
Dry cracked lips
-
No tears when crying
-
Extreme fussiness
-
Fast breathing
-
Faser than normal heart rate
-
Sunken eyes
-
Sunken fontanelle – the soft spot on top of the baby’s head
-
Skin is dry to the touch
-
Low energy levels
-
In serious cases – your little one can become delirious or unconscious (this is an emergency and not an early sign of dehydration)
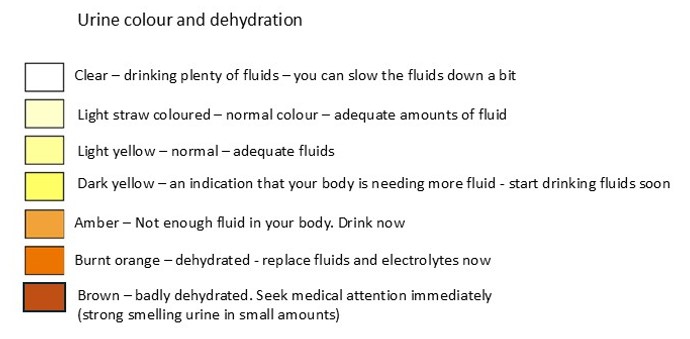
Urine colour chart
It is helpful to compare the urine (wee) colour to the colour in the chart below – it gives a bit of perspective to the degree of dehydration and what to do next!
Treat early – don’t wait
If your little one has diarrhoea – start giving rehydration solution. You can make your own solution at home. Use previously boiled water that has cooled or safe clean water.
1 litre of water (approx. 5 cups of water)
Add 8 teaspoons of sugar
Add ½ teaspoon of salt
Stir until dissolved.
Keep offering small quantities to your little one.
It is important to know that if your little one is vomiting as well. Offer very frequent small quantities to your little one. Remember even if your little one vomits again – they never vomit all the stomach contents, so some will stay down – just keep persevering! Every mouthful can make an enormous difference!
If you are breastfeeding your little one – keep offering the breast and in between times give the rehydration solution.
It is important to give the rehydration solution and not just water. Your little one needs the glucose (sugar) to replace its energy and the salt is important to keep the electrolytes balanced in his body.
When to see a doctor if your child is dehydrated
-
Your child doesn’t appear to be recovering and improving
-
If your little one is becoming more dehydrated
-
If there is blood or mucous in your baby’s stool
-
If your toddlers vomiting and diarrhoea is persistent and severe. If they are losing more fluid than they are able to take in as a replacement solution
-
If the diarrhoea is lasting more than a few days
-
Your baby has diarrhoea and is under 6 months old
-
If his temperature is greater than 38.5°C
Let’s look at something of a timeline
When the diarrhoea starts
If you are breastfeeding – continue breastfeeding on demand as well as giving rehydration solution
If not breastfeeding – continue offering food and drink and give rehydration fluids
The first 4 – 6 hours
Offer the approximate amounts of rehydration fluid depending on the little ones weight and age – use these numbers as a guideline
-
Less than 4 months / less than 5kg : 200 - 400ml in the first 4 hours
-
l4 – 11 months / 5 – 7,9kg : 400 – 600ml
-
12 – 23 months / 8 – 10,9kg : 600 – 800ml
-
To 4 years / 11 – 15,9kg : 800 – 1 200ml
-
To 14 years / 16 – 29,9kg : 1 200 – 2 200ml
-
15 years or older / 30kg or more : 2 200 – 4 000ml
If your little one refuses to take the fluid from a cup or bottle – use a syringe or a teaspoon or a medicine dropper – you can’t take no for an answer
If your little one is vomiting, give rehydration fluid 15ml (1 tablespoon) every 10 – 15 minutes until; vomiting stops
6 – 24 hours
-
Continue breastfeeding
-
Continue with the rehydration fluid /p>
-
Keep a close lookout for the signs of dehydration
-
Check the urine colour chart – make sure the colour of the urine is getting lighter and the quantity of urine is increasing
-
Stay vigilant
-
When vomiting stops, give baby his usual formula and feedings in small frequent amounts
-
After 24 – 48 hours, most children can resume their normal diet
-
It can take 7 – 10 days for the stool to be normally formed again – while the bowel is healing.
What should parents not give their child to drink?
-
Do not give sugary drinks – this will likely cause more diarrhoea
-
Do not give fruit juices, soft drinks etc
-
Do not give over the counter medication to stop the diarrhoea – as some of these prevent the body getting rid of the toxins or infection
The degree of dehydration is rated on a scale of 3
During diarrhoea – the body loses more fluid than is being replaced.
-
severe dehydration (at least 2 of the following)
-
lethargy / unconsciousness
-
sunken eyes
-
unable to drink or drinking poorly
-
skin pinch goes back very slowly (≥2 seconds)
-
-
some dehydration (2 or more of the following)
-
restlessness, irritability
-
sunken eyes
-
drinks eagerly and thirsty
-
-
no dehydration (not enough signs to classify as some or severe dehydration)
Remember
-
Don’t just look at the nappy
-
Look at the baby
-
Is your baby happy and content?
-
Has your baby had a personality change?
Lynne Bluff
BSc Nursing Wits
Registered nurse and midwife
Internationally certified childbirth educator
References
https://pmc.ncbi.nlm.nih.gov/articles/PMC2791660/
https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease
https://www.healthdirect.gov.au/diarrhoea-in-children
https://caringforkids.cps.ca/handouts/health-conditions-and-treatments/dehydration_and_diarrhea
https://www.healthline.com/health/parenting/signs-of-dehydration-in-toddlers
https://www.nhs.uk/conditions/dehydration/
https://www.ghsupplychain.org












