It is estimated that when a couple is having trouble conceiving, four out of ten times it is because of the man not producing or delivering sperm. Some men produce very few, or no sperm at all, or the sperm they do produce are abnormal. This makes sperm donation the only option for couples who are keen to have a baby.
Sperm donation can be used when:
A man has had a vasectomy previously and now wants to father a child
In same-sex relationships and for single women
Where the man in a relationship is a carrier of certain genetic diseases
When there has been previous treatment that has altered sperm production, such as radiation or chemotherapy for cancer
Where previous illness, e.g. mumps, has rendered the man in a relationship infertile
Obtaining donor sperm:
Couples may choose to do their own research among friends and family, and make their own negotiations and arrangements about sperm collection and insemination. They may choose not to use a fertility clinic at all and do their own research and conception planning.
Couples may elect to go with a fertility clinic and use donor sperm where the identity of the donor is unknown to them. Some information about the donor is made available, but identifying information such as name and address are not shared.
Another option is to use the services of the clinic to screen and organise insemination with the sperm of a known donor. The sperm is only used for one client and is the preferred option for single women who wish to conceive but who are not in a relationship.
How donor sperm is used:
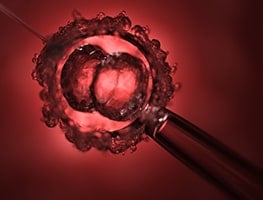
If donor sperm is arranged through a fertility clinic, it can be used via insemination or as part of an overall In Vitro Fertilisation (IVF) procedure. Artificial insemination can be a very simple treatment for infertility; however, freezing and storing sperm is much more difficult and involves more cost. If donor insemination is done, the sperm is injected directly into the woman’s womb and timed with her ovulation. If it is used during IVF, the sperm is used to create an embryo with the woman’s ova (egg) and then transferred into the womb.
Many couples worry that using donated sperm to achieve a pregnancy will affect its success. But research shows that there is the same rate of pregnancy complications from using donor sperm as there are through natural conception. Sperm donation in itself does not add to pregnancy risk.
If couples want to use sperm, which has been arranged through the fertility clinic, careful screening procedures are done to ensure it is safe to use. Most clinics limit the number of times a donor’s sperm can be used, and even where the donor is known to a couple, the same checks are done as for anonymous donors.
What’s sperm worth?
Sperm donation needs to be done for altruistic reasons and not for monetary gain. In South Africa, it is illegal to accept any payment for human tissue. The Human Tissue Act prohibits donors from selling organs or tissue, and therefore the donor is only entitled to have his expenses covered. Only samples that fulfil all the required semen parameters will be frozen. Donors are reimbursed for their time and travel costs and are not expected to pay for tests associated with the donation procedure.
Some couples choose to access sperm donation through informal avenues, such as internet web-sites. This is potentially risky both for legal and health reasons. However, for couples who cannot afford fertility treatments through reputable clinics, this may be their only option of conceiving.
Sperm donors need to meet certain criteria to qualify. Each fertility clinic has its own guidelines but generally:
Men need to:
Be aged between 18-45 years. If the donor is known then he may be older than 45 years.
Be healthy, non-smoking men.
Have at least a matric certificate, preferably with tertiary training/ studies.
Be of any race.
Understand and comply with the relevant legislation regarding sperm donation. There are clear ethical and legal responsibilities in becoming a sperm donor and it is vital that the donor is well informed of these.
Be prepared to provide genetic and family information, which could influence the child.
Provide information on previous sperm donations. This is to ensure the limit of 5 families is not exceeded.
Consent to a medical interview and check-up.
Have counselling and be prepared to provide written consent for the use of his sperm. If the donor is married or in a relationship, it is often a requirement for his partner to come to counselling as well.
Be prepared for semen to be frozen and quarantined for 3 months so it can be tested and retested prior to use. This is essential to ensure the HIV virus (in particular) is not present.
Be prepared to provide information, which does not identify him, but will help the recipient make their own informed choices about accepting the donor sperm or not.
Bring identifying information to the fertility clinic, which includes photo ID as well as his name and address.
Collection
The donor will be expected to produce semen samples twice a week. Only semen samples that are of sufficient quality will be frozen and used in the sperm donor programme. Blood samples are also required for screening every six weeks. The final blood screening will be taken four weeks after the last semen sample has been accepted.
Initial testing and analysis of the donor’s sperm is done to check whether it is suitable to use. A fresh sample is necessary to gain an accurate analysis of the number of sperm present and to analyse how it stands up to the rigours of being frozen. Donors are asked to abstain from having sex for up to three days before they provide a sample.
Every clinic has a private room which donors use to go and masturbate in and collect a semen sample. It takes 1-2 weeks before the clinic can determine whether the sample is suitable and donations can proceed.
Each clinic has their own practices but, generally, up to ten separate donations of semen are required once it has passed laboratory screening.
Medical checks:
The following blood tests must be done at the start of the donation cycle and one month after the cycle is completed:
Human immunodeficiency virus (HIV)
Sexually transmitted infections (TPHA & RPR)
Hepatitis B
The donated sperm is frozen for three months and then the HIV test is repeated. The sperm can only be used after three months to ensure the donor is not in the window period of HIV infection.
For this reason The Centers for Disease Control has cautioned that fresh anonymous donor sperm should not be used for artificial insemination or AR – the minimum 90 days quarantine is critical.
During this time screening tests are done to identify if there is any risk of passing on any genetic abnormalities.
Sometimes, sperm is not suitable for donation, but this is not obvious until it has been analysed. Some of the more common reasons for this can be:
If there is insufficient number of sperm being produced
The sperm are abnormal or carry genetically-linked disorders
If the freezing process renders them unsuitable to use
Most recipients are keen to have some say in the physical characteristics of the sperm they receive. Some choose to request sperm is stored for future pregnancies if they want to have future children with the same biological father.
Legal rights:
In South Africa the law prohibits disclosure of donor and recipient identities.
The identity of the donor shall remain anonymous and the clients have in no way the right to learn the identity of the donor or solicit donor-identifying information from any other source.
The donor is also free from any responsibility to the biological offspring produced by his sperm.
Children born from a sperm donor are not entitled to find out the identity of the donor, likewise, the donor will not receive any information regarding the recipients of his sperm and will not find out whether it resulted in a live birth.
The donor has the right to indicate whom he would like to receive his sperm, e.g. religious preference, ethnic grouping etc.
All donor sperm banks in South Africa should be registered at Health Professions Council of South Africa (HPCSA) and should have a practicing licence; therefore sperm from unlicensed sperm banks is illegal.
In South Africa a donor is limited to five births.
For more information: